|
CoQ10 is an important essential enzyme in the body that participates in energy movement via the electron transport chain, partakes in production of building blocks for DNA, and also acts as an antioxidant in cellular membranes (Casagrande et al., 2018; Fischer et al., 2011; Medline Plus, 2017; Xie et al., 2022). For humans, CoQ10 is at its greatest concentration around age 20 when it starts to decline; this decline varies for each individual based upon a number of factors including but not limited to: metabolic syndrome, Alzheimer’s disease, vitamin A deficiency, medication usage, oxidative and physiological stress, and GI absorption issues (Casagrande et al., 2018). It is often prescribed to support cardiometabolic function. For intake, CoQ10 can be obtained from dietary sources, however very little (less than 10%) is actually absorbed from these sources and this absorption is influenced further by the underlying health of the individual, especially in regard to their digestive system (Casagrande et al., 2018; Xie et al., 2022). This warrants the need for supplementation in most cases but especially in those at greatest risk for accelerated decline (Casagrande et al., 2018; Xie et al., 2022). The most bioavailable CoQ10 supplement is the solubilized form of ubiquinol, those with greatest declines should consider this form over others (Casagrande et al. 2018).
In general, 22-400 mg/day of CoQ10 supplementation is considered safe, but even in clinical trials with high dosing, the adverse effects seen were not significant enough to stop usage, therefore 100 mg/day is definitely considered an acceptable dosage for adult patients (Casagrande et al., 2018; Xie et al., 2022). Conversely, for some individuals 100mg/day may not be enough due to genetic variations, challenges with absorption, certain disease states, age, medication usage, general health, inflammation levels, and stress load; even the mitochondrial size can influence needs (Casagrande et al., 2018; Fischer et al., 2011; MedlinePlus, 2017; Xie et al., 2022). Serum levels may be needed for individualized dosing, but due to the inevitable decline of this enzyme and the relative safety of supplementation, even without lab draws, it is appropriate to recommend all adults over age 20 take a supplement form of at least 100mg/day (Casagrande et al., 2018; Xie et al., 2022). It is important to note that extremely high doses may be recommended for individuals with genetic variants, but genetic testing should be done when at all possible to confirm this need (Xie et al., 2022). References Casagrande, D., Jordao, A. A., & Waib, P. H. (2018). Mechanisms of action and effects of the administration of Coenzyme Q10 on metabolic syndrome. Journal of Nutrition & Intermediary Metabolism, 13, 26–32. https://doi.org/10.1016/j.jnim.2018.08.002 Deichmann, R., Lavie, C., & Andrews, S. (2010). Coenzyme q10 and statin-induced mitochondrial dysfunction. The Ochsner journal, 10(1), 16–21. Fischer, A., Schmelzer, C., Rimbach, G., Niklowitz, P., Menke, T., & Döring, F. (2011). Association between genetic variants in the Coenzyme Q10 metabolism and Coenzyme Q10 status in humans. BMC Research Notes, 4(1), 1–7. https://doi.org/10.1186/1756-0500-4-245 MedlinePlus. (2017, April 1). COQ2 gene. MedlinePlus. https://medlineplus.gov/genetics/gene/coq2/ Xie, J., Jiang, J., & Guo, Q. (2022). Primary Coenzyme Q10 deficiency-7 and pathogenic COQ4 variants: Clinical presentation, biochemical analyses, and treatment. Frontiers in Genetics, 12(776807), 1–18. https://doi.org/10.3389/fgene.2021.776807
0 Comments
CONSIDERING THE ROLE STRESS MAY PLAY IN EMOTIONAL EATING. WHAT ARE SOME POTENTIAL MIND-BODY INTERVENTIONS THAT MAY FACILITATE DECREASED STRESS AND BALANCED EATING HABITS?Stress can stem from a plethora of sources, and the perception of stress varies from person to person. This stress can lead to a variety of disordered eating habits, especially around emotional eating (Hernandez-Hons & Woolley, 2012; Ramos-Jiménez et al., 2015). Some individuals may have a physiological response where blood flow is directed away from the gastrointestinal tract, resulting in reduced appetite (Hernandez-Hons & Woolley, 2012). This can transition into a coping mechanism or manifest into a full-blown eating disorder (Hernandez-Hons & Woolley, 2012). Others will take the opposite tact and respond to stress by increasing their intake of certain foods, often evolving into a bingeing pattern of eating (Hernandez-Hons & Woolley, 2012; Lattimore et al., 2011). Regardless of the change in eating behavior, the influence on health and well-being is far-reaching, creating a perpetual cycle of increased stress and continued disordered eating patterns.
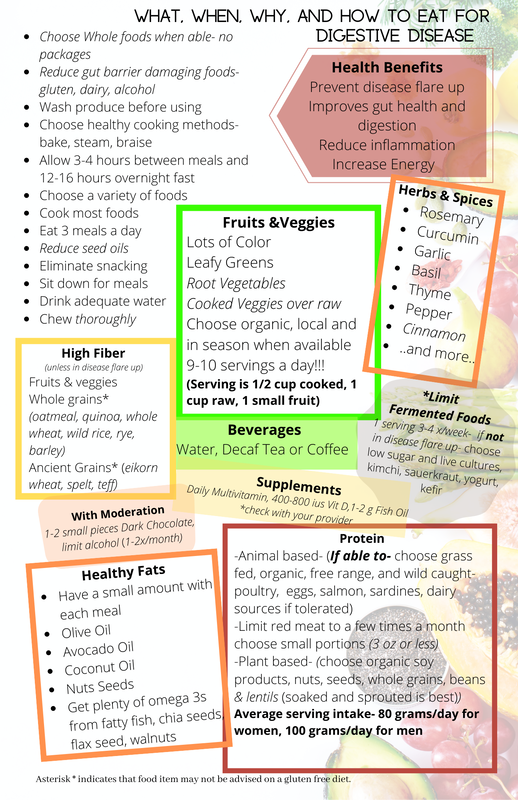
Yoga and meditation are two mind-body interventions that simultaneously decrease stress and positively influence eating behavior (Ramos-Jiménez et al., 2015; Sampaio et al., 2021; Watts et al., 2018). Meditation can help regulate the body's stress response and support anxiety management by improving self-regulation and awareness, which influences eating behaviors by increasing mindfulness around food choices and physiologically adjusting reward pathways in the brain (Sampaio et al., 2021). Yoga works in a similar fashion but also adds a physical activity element through the movement aspect of the practice, which improves awareness of nutrient and caloric needs (Ramos-Jiménez et al., 2015; Watts et al., 2018). There can also be a strong community influence from a yoga practice that provides an emotional support system to help the individual cope with stress-related challenges (Ramos-Jiménez et al., 2015; Watts et al., 2018). Yoga and meditation offer the individual an alternate method to manage stress, and just as stress and disordered eating are perpetual and cyclic in the influence of each other, so too are healthy habits and mind-body modalities. As a former colleague of mine so eloquently stated: “Eating chips, drinking beer, and sitting on the couch go really well together, but none of those go well with walking on the treadmill.” In other words, healthy habits beget healthy habits, just as poor habits beget poor habits. References Hernandez-Hons, A., & Woolley, S. R. (2012). Women's experiences with emotional eating and related attachment and sociocultural processes. Journal of Marital and Family Therapy, 38(4), 589-603. https://doi.org/10.1111/j.1752-0606.2011.00239.x Lattimore, P., Fisher, N., & Malinowski, P. A. (2011). Cross-sectional investigation of trait disinhibition and its association with mindfulness and impulsivity. Appetite, 56(2), 241-248. https://doi.org/10.1016/j.appet.2010.12.007 Ramos-Jiménez, A., Wall-Medrano, A., Corona-Hernández, R. I., & Hernández-Torres, R. P. (2015). Yoga, bioenergetics and eating behaviors: A conceptual review. International journal of yoga, 8(2), 89–95. https://doi.org/10.4103/0973-6131.158469 Sampaio, C. V. S., Magnavita, G., & Ladeia, A. M. (2021). Effect of Healing Meditation on stress and eating behavior in overweight and obese women: A randomized clinical trial. Complementary therapies in clinical practice, 45, 101468. https://doi.org/10.1016/j.ctcp.2021.101468 Watts, A. W., Rydell, S. A., Eisenberg, M. E., Laska, M. N., & Neumark-Sztainer, D. (2018). Yoga’s potential for promoting healthy eating and physical activity behaviors among young adults: a mixed-methods study. International Journal of Behavioral Nutrition and Physical Activity, 15(1). https://doi.org/10.1186/s12966-018-0674-4 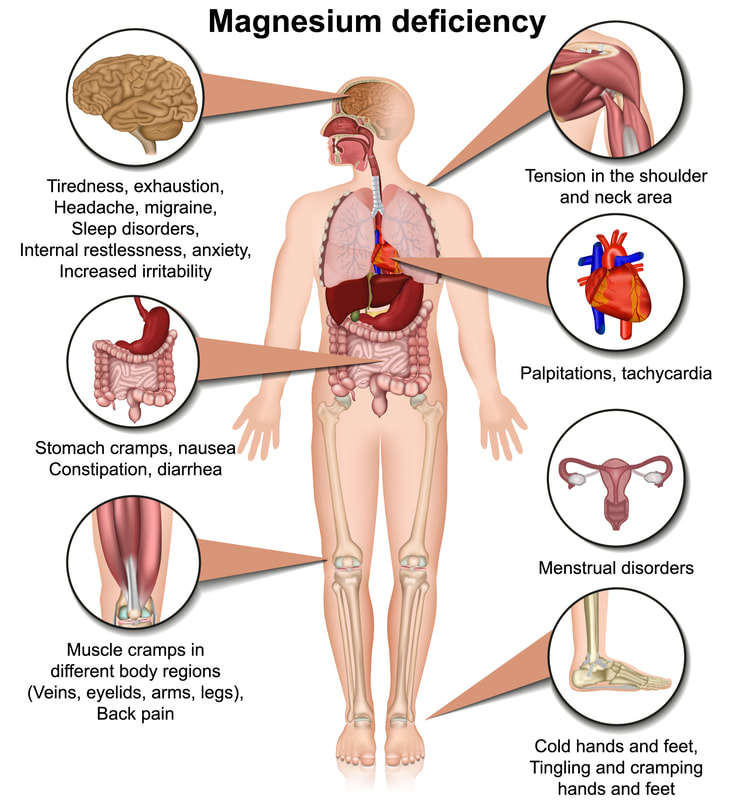 Magnesium is an important mineral that we get from the diet and is found in a diverse array of whole foods. It is a hot nutrient topic right now and for good reason. Although commonly seen in hospitalized patients, the general "healthy" population is now estimated to have a high level of deficiency that is going unchecked. This is concerning as magnesium supports many pathways and functions in the body including but not limited to: bone support, hormone functioning, blood clotting, and DNA replication (1). A deficiency could contribute to, or worsen, chronic conditions, as well as promote new health concerns. As health care practitioners it is difficult to bring awareness to this need as the symptoms of deficiency are vague: fatigue, lethargy and muscle weakness; and can easily be mistaken for other issues (1). There are also challenges in the serum reference ranges for testing and it is difficult to detect reductions of the magnesium in tissues, so baseline for supplementation can be challenging (1). The standard RDA (recommended dietary allowance) for adults is variable and depends on age and biological indicators. In general the recommendations are around 400 mg/ day which is the typical dose available in over the counter supplements (1). The good news is that magnesium is found in many foods and eating a whole foods based diet with a variety of items is a good way to meet your needs without the need for supplementation. It is important to note that food processing does diminish the magnesium content of many food items so choosing organic whole foods (if possible) is the best way to ensure you meet your needs. If you feel supplementation is still the best choice for you, talk to your provider to make sure there are no health reasons that you should not supplement. If you do choose to supplement be sure to purchase a quality product to ensure the best absorption, with nutrients and supplements quality really does make a difference. Magnesium Food List from the NIH Data Base
References
1. Gropper, S., & Smith, J. (2017). Advanced nutrition and human metabolism (7th ed.). Belmont, CA: Wadsworth Publishing/Cengage Learning. 2. National Institutes of Health Office of Dietary Supplements. Magnesium Fact Sheet for Health Professionals Accessed 05/06/2021. I receive a lot of questions about bariatric surgery and potential malabsorption concerns with it so I thought I would share some evidence around some common deficiencies and complications with those deficiencies.
Which nutrient deficiencies might cause neuropathy? The nutrient deficiencies that could contribute to, or be the cause of neuropathy are vitamin B1, B12, B6, vitamin E, and copper, which is associated with optic neuropathy (Becker et al., 2012). Vitamin B2 also causes “burning feet syndrome” which can be a sign of peripheral neuropathy (Martin, 2018). How would you differentiate which nutrients might be responsible for neuropathy? It is not always easy to isolate which nutrient deficiency is responsible for the reported neuropathy in the patient. There are several factors to consider when reviewing patients symptoms, but one major consideration is the time of the onset of symptoms, most neuropathies present years after bariatric procedure (Becker et al., 2012). Thorough review and assessment of patients diet, nutrient status, and medical history should be conducted when presented with neuropathy (Becker et al., 2012). Assessing the specifics of the neuropathy such as the time of onset and how it presents is a good starting pointing (Becker et al., 2012). Then testing for specific nutrient deficiencies and ruling out other potential causes is a good way to work on isolating which type of deficiency is present (Becker et al., 2012). Which micronutrient is most likely to show deficiency first? Thiamine deficiency usually presents within 8 – 12 weeks post-surgery but can be seen as early as 6 weeks (Becker et al., 2012). In my experience in working for a bariatric program for the last five years, in which three of those years I was the Program Coordinator, we most often saw thiamine deficiency. It was also challenging to get doctors to always identify this as the issue. One patient in particular had a history of alcohol abuse and he was often brushed off on the assumption that perhaps he had started drinking again. Thankfully he presented to the ER one day when one of the more progressive providers was working and he contacted me to discuss his symptoms and together we were able to identify thiamine deficiency. An easy blood test identified this. I have also worked with clients who did not have good medical coverage for additional lab work and their insurance providers did not cover some of the nutrient testing that I felt they should routinely have. What are the general supplement recommendations for most bariatric surgery patients? In the clinic that I worked we would routinely recommend a B complex, B12, Vitamin D, Calcium (although this is debated), vitamin C (for healing), Multivitamin, Iron (on occasion- not for everyone), and then others based on patient’s needs. From my own research I would also recommend K2, CoQ10, fish oil, and magnesium. I will say that we only performed Sleeve Gastrectomy and the surgeon I worked with INSISTED that this was not a malabsorptive procedure and therefore there was no need to supplement if patients were able to meet their nutrient needs via the diet. To support him and also do my duty as a dietitian I would confirm what he said but also reiterate the fact that they most likely will not be meeting their nutrient needs simply by the fact that their portions are so small and for many weeks they are utilizing liquid nutrients which may not be as absorbed so supplementing could help prevent deficiencies later on. Most patients agreed with this and were happy to supplement. The sleeve gastrectomy makes it easier to use any type of vitamin, but I did have a lot of clients start to look into vitamin patches per information they learned from their support groups and bariatric blogs. This is an area that I admittedly have not had the time to dive into, but I do think it is curious as we do absorb things well trans dermally. According to the text and the readings, the common supplement recommendations post bariatric surgery are vitamin A, thiamine, B12, Folate, Iron, Calcium, vitamin D, vitamin E, vitamin K and Copper (Becker et al., 2012; Litchford, 2013). B12 deficiency is common in patients aged 50 and older. Long-term deficiency can cause permanent neurological damage. B12 deficiency is missed in many patients because symptoms are vague, worsen progressively, and serum levels are a poor indicator of sufficiency. Outside dietary insufficiency, list at least two causes of B12 deficiency. Two common causes of B12 deficiency that are seen frequently by dietitians are: medication use that reduces absorption of B12, and post-bariatric surgery status (Litchford, 2013). The medications that typically affect absorption most likely to be seen in a nutrition consult are proton pump inhibitors and metformin (Litchford, 2013). Bariatric Surgery includes both the Roux-en-Y procedure and the Sleeve Gastrectomy (Litchford, 2013). Why does the risk of B12 deficiency increase with age? What is the mechanism? B12 deficiency is more common in the elderly population because there is an increased risk for a decrease in nutrient intake, and there are increased challenges to absorption of nutrients in the aging body (Litchford, 2013). Some of the signs and symptoms of B12 deficiency are more common and expected in the aging population so can be unidentified until later stages of the condition (Martin, 2018). Nutrient intake amongst the elderly is more common because of a number of factors including but not limited to; decreased appetite, chewing and swallowing difficulties, changes in tastes, access issues to healthy foods, and cognitive impairment (Litchford; 2013). B12 deficiency at its end stage is known as pernicious anemia and is the result of a prolonged reduction and loss of the synthesis of intrinsic factor which is essential for the uptake of B12 (Litchford, 2013; O’Leary & Samman, 2010). In the ageing population this can be diminished for a variety of reasons, one of which is the use of certain medications for conditions that correlate with ageing (Litchford, 2013). Which medications increase the risk of B12 deficiency? The medications that are commonly known to increase the risk of B12 deficiency are: omeprazole, lansoprazole, Tagamet, Pepcid, Zantac, cholestyramine, chloramphenicol, neomycin, colchicine, metformin, nitrous oxide anesthesia, and some epileptic medications (Litchford, 2013; Martin, 2018; O’Leary & Samman, 2010). Becker, D. A., Balcer, L. J., & Galetta, S. L. (2012). The neurological complications of nutritional deficiency following bariatric surgery. Journal of Obesity, 2012, 1-9. https://doi.org/10.1155/2012/608534 Litchford, M.D. (2013). Nutrition focused physical assessment: Making clinical connections. Case Software. Martin, C. (2018). Detect nutrient deficiencies with NFPE. Today’s Dietitian, 20(3), 42. O’Leary, F., & Samman, S. (2010). Vitamin B12 in health and disease. Nutrients, 2(3), 299-316. https://doi.org/10.3390/nu2030299 (Links to an external site.) I stepped outside today in my bare feet onto a dry spot of ground. I stood next to the dog and cat who were sharing my little dirt patch and let the sun bathe me in Vitamin D. I took off my coat and was tempted to put on a t-shirt because I was getting so warm, after all it was a balmy 35 degrees. Sounds cold if you are reading this in Florida or Mexico, but for us here in Minnesota today is a 60 degree increase in temp from a week ago. It's almost a heat wave, this sounds especially strange considering that in Texas they are in a deep freeze. This isn't the first time the weather has felt a little funny, like things were backwards or upside down. And I know I'm not the only one to notice, all you have to do is turn on the news and you are inundated with phrases like "climate change", "Paris climate accords", "sustainable resources", and "green energy", amongst many more. It seems like we have been talking about environmental concerns for a while and suddenly we have jumped head first into action. The environmental crisis debates are increasingly more challenging to follow. Suddenly there is more depth to the conversation and answers are not as easy as originally thought.
When the idea of all electric cars was presented, at first glance it seemed amazing, no emissions! Yay! But what about the mining for the material to build the batteries for those cars? What about the plethora of cars that already run on gas? Do we just throw them away? Do we convert them? What will that cost be? Would it be a better idea to reduce drivers instead and have less cars on the road? Maybe reinvest in public transportation, encourage more incentive for companies to provide work from home opportunities? Create efficient cross country train travel? More commuter friendly neighborhoods? Could we advocate for busses for after school activities to reduce 55 suburbans parked by the curb after soccer practice? Maybe encouragement for households to have one car instead of five (like we have...)? So many questions and who has the answer? The left? Maybe. The right? Maybe. Most likely its someone in the middle. What about the idea of wind and solar energy? Another fantastic dream at first glance, but look at what is happening in Texas right now. Or look at some challenges other countries utilizing wind power have faced. Sometimes there is no wind. What do you do then? Build bigger more efficient batteries to store power for those times? Great! More mining for batteries. Maybe create a hybrid blend of energy: wind/electricity/fossil fuels/solar? Another great idea but maybe a little overkill and what would it take to switch back and forth, how much manufacturing would have to go into create a system for that switch? Maybe not that practical of a solution and certainly not accessible for all nations. Maybe we could be a little less dependent on energy to being with? On a sunny day could we keep all the lights off? Could we build houses with windows that are strategically placed to allow sunlight to be the primary light source all day long? Could we tolerate a slightly lower temperature in our house during the winter and a slightly higher temp in summer? Could we go a whole day without using any electricity? Who has the answer to this challenge? The left? Maybe. The right? Maybe. Most likely its someone in the middle. What about agriculture? How do we solve this problem? More genetically modified crops? Less genetically modified crops? Should we eat less meat? Should we garden more? Should we subsidize farmers? What about overfarming and stripping the land of its resources? Can we just put some resourced back in there? Or do we need to let the land rest? Could we continue to rotate crops or could we get creative and find a cycle of animals and crops? Could we let sheep graze in a crop field one season and then let chickens pick and poop their way through it the next? Could we create more urban green space? Could we teach individuals how to garden in their apartments? Would that require more energy? More resources? Is the payoff worth it? Maybe we could just eat less food? It probably wouldn't hurt. So. Many. Questions. And honestly there is probably not one right answer. The key to saving our planet is going to be multi-pronged and going to be a work in progress. The biggest question I have and the biggest question I don't think is addressed is: What can I do?? What can the individual consumer do?? How do we make a change that has impact and meaning? Maybe we can't afford to convert our house to solar energy and maybe we don't agree with the logic. We don't have to make or be part of big industrial change, perhaps we will be and perhaps we will all be forced at some point to do these things, but for now there are some very simple and easy things EVERYONE could do to make a difference.
Try a few or try all of these ideas. Figure out what works for you and just do it. Encourage your friends and family to do the same. Teach your kids to enjoy the natural light, teach them how to fix things so they have that skill, teach them efficiency. Share with friends and co-workers. Suggest a walk to the store to run errands with a coworker over lunch (if your location permits). Just do something. Too often we are plagued with the idea that our efforts don't matter. They do. Especially if we all do something. I think Im going to start with the lights out snuggle time :). I like the immediate benefits of that effort... How about you? What will you change? Share privately or in a comment if you want, I would love to hear from everyone. Disclaimer- This article is ENTIRELY opinion based, not fact based. It is my personal feel on things and is in no way a claim that this is how others feel, manage or navigate being ill.
It’s hard to log onto to any type of internet platform without seeing recommendations for what to do with all things COVID related. In fact, I did a quick review and in under 5 minutes I found a variety of opinion and evidence-based articles sharing data, tips, or general recommendations on how to navigate through our newest viral instigator. Information on how to quarantine… how to order food online… what supplements to take… what healing remedies to implement… what OTC meds to take… which OTC meds to avoid…. how to apply for unemployment… how to talk to your kids during quarantine… how to talk to your boss during quarantine… how to tell others that you have COVID…. how to keep the household uplifted during quarantine…the list goes on. To say we have ample support for what to do if we get COVID, if others have COVID or how to manage in quarantine, is an understatement. But what happens if we have a regular run of the mill cold? What if we or our kids come down with Strep throat? What if a coworker is coughing while at work because of her asthma? What if the dry air in our homes is making us have a sore throat in the morning? What if a parent comes down with pneumonia UNRELATED to COVID? What do we do? How do we navigate these other conditions that didn’t go away when COVID came? What do we say to ourselves and others? What do we do when it isn’t COVID? I had the opportunity to be in this space this past week and I can say I was unprepared and overwhelmed by the enormity of how to navigate. We had an outbreak of strep throat in our home. I can say I never thought I would utter the words “Oh good..” when the nurse called with the positive strep results. But here we are, in a time when we are grateful for what we know and overly cautious of what we don’t. In the past I would simply have told friends, family, and clients that my daughter was sick, and I too am not feeling well. I would have made the decision to cancel clients, call in sick or stay home based on whatever symptoms we had and whether we were contagious, as well as what my own body said it needed. I would then do what needed to be down and most likely have made the decision to lay low, stay home, and give my body time to heal. But that path didn’t feel good enough. Being sick in this COIVD era is no longer a personal experience and an opportunity to be responsible for yourself, it is now a public health matter. And depending on how much interaction you have in the community and what you do for work, it can be an absolute nightmare. I found myself acting in such uncharacteristic ways. For example, at one point I was googling whether I needed to “quarantine for strep”… Ummmmm WHAT?!? I am more rationale than this, but I was doing it all the same. Then when I finally reached out to my clients, I shared a longer than necessary explanation either over the phone or via text about why I was cancelling classes or sessions, and I felt the need to assure them, in an annoyingly high multitude of ways, that NO we did not have COVID. I made sure to obtain documentation from the doctor to share with school, work, or anyone else that may have need of it. I was overanalyzing every symptom any of us had. I became obsessive about checking temperatures of everyone despite no one at any time having a fever. I agonized over how to call in sick to the hospital I work at once a week, I worried if I stayed home one day, they may require a 14 day quarantine no matter what (this isn’t there policy and I know this, but the irrationality was thick at this point). I even debated dosing up on meds so that no one would know I was sick, and I could continue with none the wiser (obviously not a good plan but again, please note the irrational state I had sunk to). In general, my anxiety had tripled from its usual elevated stance and it was trickling down to everyone else. My daughter started to apologize if she coughed and she began to do hourly temperature checks on herself. My husband and I even started bickering as I agonized, and beat to death, how to call in sick. He was tired of hearing how hard this was, and I was tired of saying it, and yet I couldn’t stop myself. Suddenly I had lost all skills for how to be sick and I was slipping into a very unhealthy and irrational management of it all. Thankfully I had a breakthrough on Friday. I had finally cancelled the last remaining client commitments for the week, a private client Friday night and a private yoga class for Saturday morning, and in completing that task, I received the most incredible sense of relief I have ever felt in my life. It was like suddenly my worries melted away. Suddenly it was ok to be sick, t was ok to rest, and it was certainly ok to recover. It was alright to not have all the answers, I didn’t need them, I just needed to release my obligations to the rest of the world for a short period of time. I was so worried about how clients would react to me being sick or to my cancelling classes that I forgot that sometimes it doesn’t matter. Sometimes we must do what’s best for ourselves and allow others to do the same. So, what do we do if it isn’t COVID? What do we do without the step-by-step guidance that we have been groomed to look for? In my opinion and from this limited experience, I feel that we need to get back to trusting our instincts and let go of what the world expects. Of course, we need to be responsible and mindful of others, but we also need to remember to listen to our bodies’ needs. In fact, DON’T do what I did and agonize over what people will think of you in how you handle yourself. Just do what’s best for you, your family and those around you. I can’t promise things will always be fine or that others will be ok with your decisions, but it will release you from an extra dose of stress which is not conducive to getting better. I felt the relief that I felt because I had finally given myself permission to get better, I was no longer trying to hide being sick, or beat myself up for being sick, instead I had accepted it and allowed myself the opportunity to be well again. Maybe this is one thing, among many, that COVID has taught us; to take a step back when our body demands it. But there are still things we need to learn. Like how we set aside our judgement and regain trust. This is not only regarding the judgement and trust of, and for others, but also how we apply these to ourselves. We must trust if someone says they have a cold that they have a cold. We must let go of judgement when we hear a cough from someone during a meeting. We must trust our own body when it says “rest”, or in many cases screams “TAKE A BREAK!!!” And finally, we must learn to take responsibility for ourselves and for our own health. This is what we do when we don’t have COVID, but surprise, surprise, this is what we also do when we have COVID… Moral of the story, take care of yourself, don’t worry about what everyone else is doing or thinks, manage your own health and that of your family and see how your sense of wellbeing slowly improves. This morning, as is usual on a Sunday in our house, I was compelled to stop my work tasks to address the ever-growing pile of dishes. I often grumble about the kids not helping or my husband conveniently occupying himself with other tasks, but today I found myself unexpectedly in a mindful state of existence. The warm water on my hands, the inability to multitask, the quiet as the household vehemently avoided the kitchen in the event I would petition for help, the scent of the lavender soap, and the sense of accomplishment as I scrubbed pans that had been sitting for the entire weekend. Watching them glisten as I scoured them clean with steel wool.
According to Merriam-Webster, the Definition of mindfulness states: 1: the quality or state of being mindful 2: the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis also: such a state of awareness Does this definition say it is only when we are sitting in a quiet corner of our house, our legs crossed in meditation? Does it say that it only happens when we read a “mindfulness” book? Is it only when we do one of the tasks our favorite podcaster lists as acceptable mindfulness tasks? Or is it only when our app tells us it is time to be mindful? Maybe it isn’t this or that, maybe it’s all the above and then some. It is in those little moments, the in between, the time that you are waiting in the exam room for your doctor and you aren’t on your phone because you don’t want to have to put it away when he/she walks in. Or maybe it’s in your evening shower, as you feel the warm water rain over your body and the worries of the day wash down the drain. Or perhaps it’s when we are walking to get the mail and see a squirrel run out with some sort of snack in his mouth. You smile at the unexpected cuteness and welcome feeling of joy you get as your soul appreciates the life of another being. Or could it be when you are standing at the sink, looking out the window at the snow-covered yard, up to your elbows in hot soapy water, your thoughts quiet and contemplative, the world quiet around you, and you are simply washing the dishes? Wherever and whenever you find yourself in these treasured moments, take a minute to appreciate the opportunity. Be happy your kids don’t keep up with dishes, so you GET this profound opportunity to do them. Be thankful your husband forgot to grab the mail on his way into the house the night before so you COULD make an excuse for a walk. Be filled with joy that your doctor is running a couple of minutes behind affording you the rare opportunity to sit longer in a space of healing and wellbeing. Mindset or Mindfulness, you oversee when you get to experience either, so instead of lamenting that your life is too crazy and busy, make the most of the times when things take a pause and show a little gratitude. I promise things always go better when we have a heart full of joy. Plus, nothing makes you feel accomplished like cleaning a sink-full of dishes. Merriam-Webster.Mindfulness.Merriam-Webster.https://www.merriam-webster.com/dictionary/mindfulness. Here is a letter that I wrote to my clients this week, so many commented how much it meant to them that I decided to share it with a wider audience. As I wrote this letter I felt like I was writing a bit to myself and I didn't realize how therapeutic it would feel. Because of this, I encourage you to take my same step, write a letter to "someone" about how things are, how you feel, thoughts, concerns, whatever comes to mind. Then feel free to send it or just rip it up. Either way, I promise you will feel better. Good Afternoon,
I wanted to take a minute and check in with everyone. It has been a while and I miss everyone. Although the studio is beginning to awaken, there are many faces I have not seen in some time. I hope you all are doing well, not just surviving, but thriving if that's possible. We are living in tumultuous times which is not news to anyone. Lately I often feel like quoting Dickens... "It was the best of times, it was the worst of times..." And this is how it feels right now. There are so many challenges that we are facing each and every day, yet at the same time there is opportunity woven in there as well. We often need a reminder of this though as the challenges take center stage and it is easy to overlook the good. As we come into the season of Thanksgiving I want to invite you to take the opportunity to focus on some silver lining moments that you have had through our COVID/election year. What are the changes you have had to make, either by choice or necessity during this time? How have they impacted your mental and physical health? If all you can think of is negative, switch your mindset and ask yourself 'What have I learned during this?' Maybe you don't see a glowing "perk" but if you examine what you have learned then perhaps you can see some benefit in that. I, for one, have learned a lot of lessons during this time and I am still being educated in many areas. In addition, here is a reminder to take care of yourself. I know that you are hearing this a lot and your response may even be along the lines of "easier said than done" and I hear you. In fact I am there with you. There are more times than I care to admit that I spend sitting in a state of fear and worry. Keeping our sanity during times like these requires more than just a bubble bath and glass of wine (although those do sound fantastic). It requires us to go a little deeper. It requires us to move into a state of non-judgement, non-judgement towards ourselves and non-judgement towards others. Judgement is an easy outlet right now. We can point fingers and blame for the pain and hurt we feel. But what would happen if we all took a moment to think through our response in a situation rather than reacting. This isn't just to others, its also to ourselves. It is said that when we judge we are just looking in a mirror. Moving into non-judgement can be as easy as showing more kindness to yourself. The effect will be 10 fold. In fact, this is where the real work happens. As you work through these thoughts remember, you don't have to do this perfectly. In fact I wouldn't expect any of us to ever be perfect. That's the beauty of this life. We are constantly growing as a person, evolving into a higher state of being. There are many bumps along that road. And remember when all else fails, go to your mat. Maybe you just sit there, maybe you practice, maybe you take a nap. But continue to go back there. Build that consistency. Experience that grounding. Find your peace. Have a wonderful week! Namaste- Jessica |
Details
Archives
June 2024
Categories |
|
Jessica Carter MS, RD, LD, CDE, RYT200 1900 Division ST W, Unit 4, Bemidji 218-556-9089 |
|
Copyright © Core Health & Nutrition, LLC.








 RSS Feed
RSS Feed